12 weeks between Pfizer jabs increases Covid immune response in over-80s
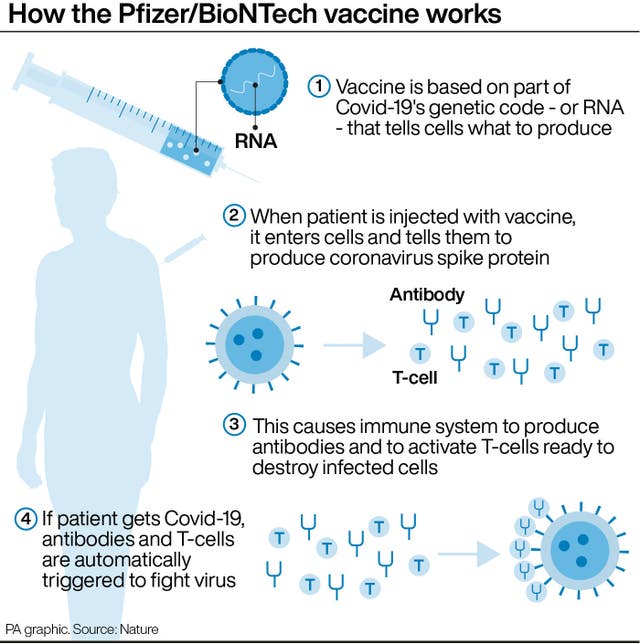
Although the Pfizer/BioNTech vaccine was originally authorised for a three-week interval, the UK extended it to 12 weeks.

A 12-week gap between Pfizer/BioNTech coronavirus vaccine doses significantly increases the immune response in older people, research suggests.
The antibody response in people aged over 80 is three and a half times greater in those who have the second dose after 12 weeks, compared with a three-week interval, the study found.
Researchers said the study of 175 people, who were older than 80 and living independently, is the first direct comparison of the immune response in any age group for the different intervals.
While the Pfizer jab was originally authorised for a three-week interval between doses, several countries including the UK extended it to 12 weeks so a greater percentage of the population could receive one dose quicker.
The study, led by the University of Birmingham in collaboration with Public Health England, found that extending the interval to 12 weeks increased the peak spike-specific antibody response to the virus 3.5-fold compared with those who had the second vaccine at three weeks
Although the peak cellular immune responses were lower after the delayed second vaccine, responses were comparable between the groups when measured at a similar time point following the first dose, researchers found.
They concluded that waiting 12 weeks to administer a second Pfizer jab potentially enhances and extends antibody immunity.
This is believed to be important in virus neutralisation and preventing infection.
First author Dr Helen Parry, National Institute for Health Research academic clinical lecturer at the University of Birmingham, said: “Sars-CoV-2 vaccines have been remarkably effective in providing large-scale protection against infection and symptomatic disease – but many questions remain regarding their optimal delivery for provision of effective and sustained immunity.
“This is the first time antibody and cellular responses have been studied when the second vaccine is given after an extended interval.
“This research is crucial, particularly in older people, as immune responses to vaccination deteriorate with age.
“Understanding how to optimise Covid-19 vaccine schedules and maximise immune responses within this age group is vitally important.”
Corresponding author Paul Moss, professor of haematology at the University of Birmingham and principal investigator of the UK Coronavirus Immunology Consortium, said: “The enhanced antibody responses seen after an extended interval may help to sustain immunity against Covid-19 over the longer term and further improve the clinical efficacy of this powerful vaccine platform.
“Our research findings may be important in the development of global vaccination strategy as extension of interval of the second vaccine dose in older people may potentially reduce the need for subsequent booster vaccines.”
Researchers analysed blood samples after participants’ first vaccine and then again two to three weeks after the second dose.
Of the cohort, 99 participants had the second vaccine at three weeks, while 73 waited 12 weeks.
Spike-specific antibodies were detected in all participants after the second dose, regardless of the gap between jabs.
However, after the second vaccine the average concentration of antibodies was 3.5 times higher in the 12-week interval group (4,030 U/ml) compared with the three-week interval group (1,138 U/ml).
Looking at the T cell response – which plays an important role in supporting and maintaining antibody production – researchers found that 60% of the three-week group had a confirmed cellular response at two to three weeks following the second vaccine, although this fell to only 15% eight to nine weeks later.
The proportion of participants showing a cellular response in the 12-week group was 8% at five to six weeks after the first vaccine, rising to 31% two to three weeks after the second.
Dr Gayatri Amirthalingam, consultant epidemiologist at PHE, said: “The higher antibody responses in people receiving two doses of the Pfizer vaccine using an extended 12-week interval provides further supportive evidence of the benefits of the UK approach to prioritise the first dose of vaccine.
“This analysis shows better antibody responses in those receiving their second dose at 12 weeks compared to the standard three-week schedule.
“It is vital that you take up the offer of vaccination as it is the best way to protect yourself and your community and to help us out of the pandemic.”
The experts say further research is required to explore these variations.
However, the researchers stress it is not possible to make a direct extrapolation from the antibody data to the real world data in terms of clinical protection.
So while the data suggests additional protection from the second dose, it is not three times as much based on the antibodies,
Prof Moss said: “The real world evidence is in terms of protection against severe disease, it is extraordinarily powerful even after one vaccine.
“There is an extraordinary boost after two vaccines in terms of measurement to the antibody response, but the clinical protection after one is very strong.”
He added that it would be fascinating to see how antibody levels wane depending on the dosing schedule, and this could have an impact on the need for a booster jab and might provide protection against coronavirus variants.
The research, published as a preprint not yet peer-reviewed, was jointly funded by UK Research and Innovation and the National Institute for Health Research, and supported by the British Society for Immunology and UK Coronavirus Immunology Consortium.