Patients ‘could be asked to travel for care’ under backlog recovery plans
The NHS is drawing up radical plans to tackle the record backlog of care.

Patients could be asked to travel for pre-planned hospital treatment in a bid to help the NHS deal with the record backlog of care, NHS Providers said.
The number of post-operative follow-up appointments could also be cut under plans being drawn up to deal with the waiting list.
Some “radical ideas” are being put forward as part of the plans, said Chris Hopson.
But the chief executive of NHS Providers said that it is more likely that people will be asked to go to neighbouring hospitals rather than different parts of the country.
NHS chiefs also faced calls to come up with an emergency plan to support ambulances services over winter as all ambulance services in England are operating on the highest level of alert.
The Liberal Democrats said that all 10 ambulance trusts in England were at the highest alert level – Level Four – on October 22 as it called for action to tackle pressures in emergency care.
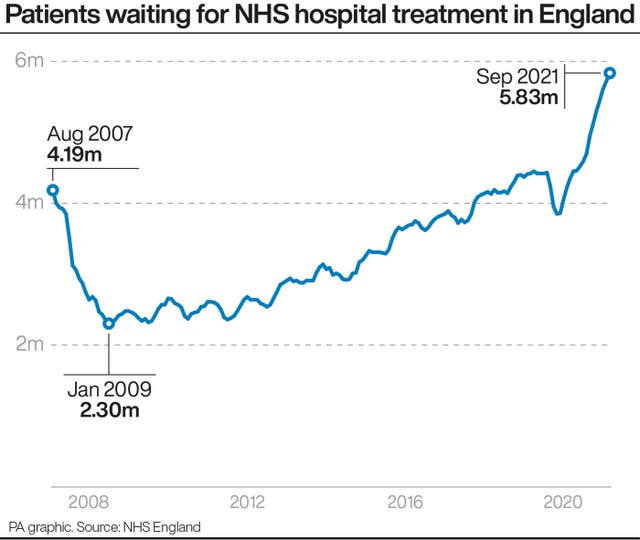
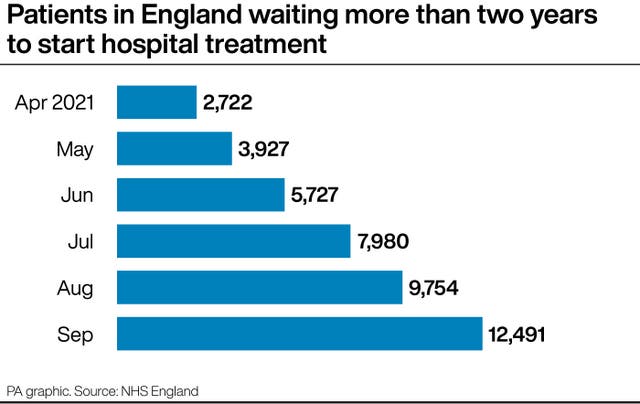
It has been reported that NHS bosses have been ordered to produce a plan for tackling the waiting list – which currently stands at 5.8 million people in England – before the end of the month.
Mr Hopson told Times Radio: “Everybody across the NHS recognises that having patients wait for their care is not an acceptable situation.
“There is a moral obligation on trusts and their leaders to make sure that they do everything they can, no stone unturned, to get through those care backlogs as quickly as possible.
“What we’re working on at the moment is a really comprehensive plan to get through those backlogs as fast as possible.
“And some of it will be all the traditional things that we do, which is: we will expand temporary capacity; we will ensure that we use overtime as much as possible; we will ensure that we use the capacity that sits in the independent sector.
“But I think we recognise we need to go further and that’s why, some of those radical ideas, we are considering and looking at them.”
He said he does not think people will be asked to travel from “Durham to Dunstable”, adding: “So, what I think will happen is that, by getting trusts to work together more effectively – as they’ve been doing over the last 18 months – you can see people being asked to be moved, you know, relatively short distances.”
Mr Hopson continued: “So if you look back to the Easter Bank Holiday, there are three trusts that are currently working together – Bath, Swindon and Salisbury.
“Bath had a significant number of children who had been waiting for a very long period of time for ear, nose and throat surgery, but because they were working together, there was some spare places in Salisbury and they wrote to all of the parents of those children and said: ‘would you like to go to Salisbury on a bank holiday weekend?’.
“What really surprised the chief executives in those trusts was that actually they had a very, very high take-up.
“So, as I said, it’s not the impression that has been given – is it sort of one end of the country to the other? No. Actually, it’s likely to be hospitals that are kind of close to each other.”
On the prospect of reducing the number of outpatient appointments following surgery, he added: “Our clinicians manage clinical risk and nobody is going basically to suggest to a patient who might have a risk ‘Oh, no, we don’t need to see you, off you go’, and ‘Actually, we’ll only see you if it turns into an emergency’.
“That is absolutely not what’s going to happen.
“The way the outpatient system tends to work in lots of specialties is that we do say to people ‘Come back in three (months), come back in six, come back in nine, come back in 12’, and, actually, you won’t need all of those four appointments in many cases.
“And moving towards a system where you can give patients the opportunity to say ‘Actually, I’ll only do the six, but if I’ve got a problem at the three in the nine-month period, I know I can get hold of you’.
“Then that will free up a lot more capacity for those consultants to actually do elective surgery and backlog recovery.
“The implication that we’re suddenly just going to say to everybody ‘We don’t want to see you anymore’ – absolutely not. It will be risk-based, as it always is, and that’s what our clinicians are brilliant at and they’re really good at identifying when they need to ask people to come back.”
NHS boss Amanda Pritchard said that one of the top priorities in the NHS is to tackle the backlog.
“(We have a) priority to do everything we can to build on the momentum we’ve already seen on recovering services which were unavoidably disrupted by Covid, particularly tackling the backlog in elective care,” she told the National Children and Adult Services conference.
“And that’s to get people, particularly those with the highest needs, seen and treated as quickly as we possibly can.
“Clearly we can go faster on that if we keep Covid cases low through the vaccine programme, and by helping more people stay well at home.”
“You will be aware I think that the Secretary of State told Parliament earlier this month we will be shortly setting out a multi-year plan to address this.
“So you’ll be hearing more about it over the coming days, weeks and months.”
The comments come as the Liberal Democrats called for action over the severe pressure facing ambulance trusts after a response to a written question in Parliament revealed that on October 22 all ambulance services in England were operating on the highest level of alert.
Lib Dem health spokesperson Daisy Cooper said: “We’re talking about loved ones waiting for ambulances that arrive too late or get stuck in queues at hospitals with devastating results.
“The Prime Minister must get a grip of this crisis instead of trying to hide it.”