Scientists develop ‘game-changing’ antibody tests to detect new Covid variants
Discussions are already underway to explore a possible rollout of the tests to the NHS.
Scientists have developed “game-changing” antibody tests that can detect whether people have been exposed to new variants of Covid-19.
Researchers said the new tests can detect antibody responses to infection by SARS-CoV-2 virus with more than 98% accuracy and 100% specificity, in contrast to currently available tests which are around 60-93% accurate and cannot differentiate between unique variants.
The new tests can be used to estimate the prevalence of circulating variant strains in the community, including the Alpha and Delta variants which were first identified in Kent and in India respectively.
Scientists said the tests have the potential to “dramatically change the trajectory of recovery” from the pandemic.
The tests can assess the long-term immunity of an individual and whether immunity is vaccine-induced or is a result of previous exposure to the infection.
They can also provide information that can be used to estimate how long immunity provided by the vaccine lasts as well as the effectiveness of the vaccine on emerging variants.
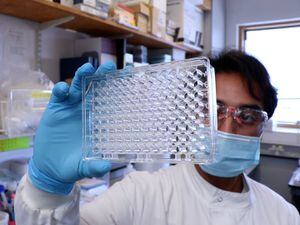
The tests have been developed by the University of Aberdeen in collaboration with biotechnology group Vertebrate Antibodies Ltd and NHS Grampian.
Professor Mirela Delibegovic, from the University of Aberdeen and academic lead on the project, said: “Accurate antibody tests will become increasingly important in the management of the pandemic and this is a truly game-changing technology with the potential to dramatically change the trajectory of global recovery from the pandemic.”
She added: “As we move through the pandemic we are seeing the virus mutate into more transmissible variants such as the Delta variant whereby they impact negatively on vaccine performance and overall immunity. Currently available tests cannot detect these variants.
“As the virus mutates, existing antibody tests will become even less accurate hence the urgent need for a novel approach to incorporate mutant strains into the test – this is exactly what we have achieved.
“Looking ahead, discussions are already underway to explore a possible rollout of the tests to the NHS which we hope to see happen soon.”
Professor Delibegovic worked alongside industry partners, Vertebrate Antibodies Ltd and colleagues in NHS Grampian to develop the new tests using the innovative antibody technology known as EpitoGen.
The team, funded by the Scottish Government Chief Scientist Office Rapid Response in Covid-19 (RARC-19) research programme, used artificial intelligence called EpitopePredikt, to identify specific elements, or “hot spots” of the virus that trigger the body’s immune defence.
The researchers were then able to develop a new way to display these viral elements as they would appear naturally in the virus, using a biological platform they named EpitoGen Technology.
This approach enhances the test’s performance meaning only relevant viral elements are included to allow improved sensitivity and this approach is capable of incorporating emerging mutants into the tests, thus enhancing the test detection rates.
Dr Robin Brittain-Long, consultant in infectious diseases at NHS Grampian and a member of the research team, said: “This new testing platform adds crucial sensitivity and specificity to the current available serology tests and has the potential to monitor individual and population based immunity in a way that has not been possible before.
“In my work, I have experienced first-hand the detrimental effects this virus can have on people, and I am very excited to add another tool in the toolbox to fight this pandemic.”
The EpitoGen platform can also be used for the development of highly sensitive and specific diagnostic tests for infectious and auto-immune diseases such as Type 1 Diabetes.